What is Living donor liver transplant ? (LDLT)
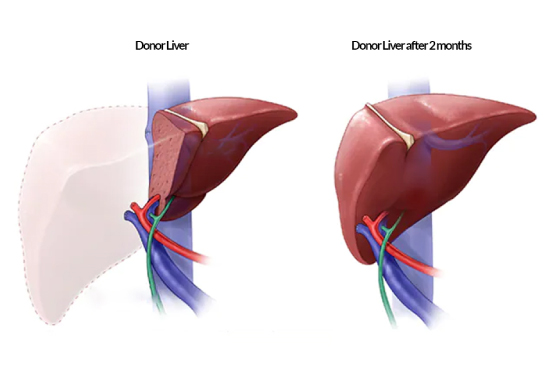
Living donor liver transplant is a surgical procedure in which a portion of a healthy liver is removed from a living donor and transplanted into a recipient with end-stage liver disease or acute liver failure. It offers an alternative to deceased donor liver transplantation when a suitable deceased donor organ is not readily available or waiting period is long. The donor operation is entirely safe and the half liver quickly regenerates in both the donor and the recipient in a few weeks. In the first few days after operation even when regeneration is not complete, the half liver is enough to maintain normal donor functions due to the immense reserve in the liver.
Who can be a living liver donor?
- The person must donate of his/her own free will
- The person should be between 18-55 years age
- The person must be a close relative.
- The donor and recipient blood group must match.
- The donor liver structure / function, as well as the other systems must be normal.(Based on the donor blood tests and scanning )
- Half of the donor liver must be enough in volume for the recipient weight. (Based on donor CT scan)
What is matching blood group to be donor for liver transplantation ?
Matching Blood Group or Who Can Donate the Liver
Patient Or Recipient
- A
- B
- AB
- O
Donor
- A+ A- O+ O-
- B+ B- O+ O-
- A+ A- B+ B- O+ O- AB+ AB-
- O+ O-
How living liver donor evaluated before living donor liver transplantation ?
Once the potential donor express the interest to donate part of his/her part of liver to her relative, the transplant surgeon carry out the following steps. The evaluation process for a living liver donor typically involves several steps to ensure the donor’s suitability for donation and to prioritize their safety. General outline of the steps involved in the living liver donor evaluation:
The potential donor initially contacts the transplant center expressing their interest in being a living liver donor. They will undergo an initial screening where they provide basic information about their health history, relationship to the recipient (if applicable), and any potential risk factors or contraindications.
The donor will undergo a detailed medical history interview, including information about previous surgeries, medical conditions, medications, and lifestyle habits. A comprehensive physical examination will also be conducted to assess the donor's overall health and to identify any potential issues that may affect the donation process.
The donor will undergo a series of blood tests to assess their blood type, liver function, kidney function, viral infections (such as hepatitis and HIV), and other factors that may affect their eligibility for donation.
Imaging tests, such as ultrasound, CT scan, or MRI, will be performed to evaluate the donor's liver anatomy and ensure the liver is suitable for donation. These tests help determine the size, structure, and blood vessels of the liver, which are important factors in the donation process.
A thorough psychosocial evaluation is conducted to assess the donor's mental and emotional well-being, their understanding of the risks and benefits of donation, and their motivations for donating. This evaluation helps identify any potential psychological issues or concerns that may impact the donor's ability to cope with the donation process.
The donor will meet with various members of the transplant team, including hepatologists, transplant surgeons, nurses, and social workers. They will discuss the details of the donation process, potential risks and complications, expected recovery, and long-term implications. The donor will have the opportunity to ask questions and clarify any concerns during these meetings.
The donor will receive detailed education about the living liver donation process, including the surgical procedure, postoperative care, recovery expectations, and the potential impact on their own health. They will be provided with information to make an informed decision about proceeding with donation.
The transplant center's multidisciplinary donor selection committee reviews the donor's medical and psychosocial evaluations, test results, and the overall suitability for donation. The committee carefully assesses the risks and benefits of donation and makes a final decision on whether the donor is approved for donation.
It’s important to note that the donor evaluation process prioritizes the safety and well-being of the potential donor. If any concerns or issues are identified during the evaluation, the transplant team may recommend against donation to protect the donor’s health.
What happens during living donor surgery?
During living liver donor surgery, a portion of the donor's liver is surgically removed for transplantation into a recipient. Here is a general overview of the procedure:
The surgeon identifies the plane of liver division, where a line is drawn to separate the portion of the liver that will be donated from the remaining liver. The resection may involve removing a specific lobe (right lobe or left lobe or left lateral lobe)
The bile duct, which carries bile produced by the liver, is carefully divided to separate it from the liver.
The surgeon takes measures to control bleeding from the cut surfaces of the liver and carefully checks for any leaks. Once satisfied with the hemostasis, the incisions are closed with sutures or staples.
Simultaneously or shortly after the donor surgery, the recipient’s diseased liver is removed, and the donated portion is transplanted into the recipient.
Following the surgery, the donor is closely monitored in the ICU for one or two days followed by 3 to 4 days in ward. Pain management, monitoring for vitals oral feed, mobilization and regular follow-up assessments are conducted to ensure the donor’s well-being and recovery.

What is the immediate post operative care of donor after the discharge from hospital ?
Two things need to be managed after discharge from hospital. One is pain, which will be taken care by oral tablets and can be stopped within 3 to 4 days after discharge. Other one is surgical wound dressing. Donor has to meet the surgeon once after 3 days from discharge and second time 7 days after the discharge. After 7 days donor can go back to their routine work. Donor is advised not to lift heavy weight and drive any vehicle for about six weeks. There will be no other restriction. Donor doesn’t require any life long test or medicines.
Are there any long term effects on the donor?
There are no long term effects on donors including physical, psychological and sexual health.










