When is liver transplant recommended?
Liver transplantation is a surgical procedure performed to remove a diseased or injured liver from one person and replace it with a whole or a portion of a healthy liver from another person, called the donor.
A liver transplant is recommended when a person’s liver no longer functions adequately enough to keep them alive. Liver transplantation is recommended when the MELD score is more than 15 or When patient start experiencing frequent attacks of liver cirrhosis related complications ( Explained in liver cirrhosis complication section) like water accumulation in abdomen (Ascitis), Kidney damage, recurrent bleeding from varices, hepatic encephalopathy, recurrent hospital admissions, loss of muscle mass and recurrent infections. A successful liver transplant is a life-saving procedure for people with liver failure.

What are the common conditions that cause someone to need a liver transplant?
Where do donated livers come from?
There are two sources of new liver
Living Donors
Diseased Donors
What is a living donor liver transplantation or LDLT?
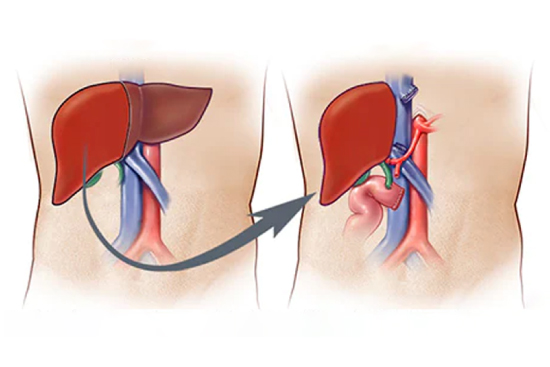
During a living donor liver transplant, a portion of a healthy person’s liver (the donor) is removed and transplanted into liver failure patient (the recipient) to replace their unhealthy liver. Both the donor’s and recipient’s livers will regrow over the next few weeks to reach normal size. Receiving a living donor transplant reduces the amount of time a person needs to wait on the transplant waiting list and hence provide higher chances of survival. LDLT is the most common form of liver transplantation in India. (More details available in next section)
What is diseased donor liver transplant or DDLT?
When the relatives of a brain dead patient agree to donate the organs, the organs including liver is harvested and implanted into liver failure patient. (More details available in next section)
What is Pre-transplant evaluation or workup? (Liver Transplant Assessment)
The liver specialist usually suggests this evaluation once patient requires liver transplant and liver transplant is planned. Recipient evaluation is done in three phases and normally takes 2-3 days. Pre transplant work up is done for following reasons.
- To establish definite diagnosis, determine the severity of liver disease and the urgency of the transplant.
- To determine the fitness of the patient for a transplant. The other systems such as heart, lungs, kidneys, blood counts are tested and the presence of any infection is ruled out. The liver specialist then decides how successful the surgery is likely to be depending on the status of the patient and the cause and severity of liver disease.
- The final phase entails the psychological and mental preparation of the patient. The patient and the family are counseled about the procedure, hospital stay, the likely course after surgery, follow up and aftercare.
- After evaluation, the patient is either placed on the waiting list for cadaveric donation, or , if there is a willing and blood group matched family donor available, he/she is evaluated for donation and a transplant is scheduled within few days.
- While on the cadaver waiting list, the patient follows up with the Transplant Team until a suitable liver becomes available. If the patient's condition shows signs of deterioration, we normally recommend the family to consider living donor liver transplant.
Anesthesia
Disconnection of Blood Vessels
Implantation of the Donor Liver
What happens during transplant surgery?
During a liver transplant surgery, a diseased or damaged liver is replaced with a healthy liver from either a living donor or a deceased donor. The procedure generally involves the following steps:
Incision
Preparation of the Donor Liver
Testing and Recovery
The length of the surgery can vary depending on various factors, including the complexity of the procedure and the patient’s condition. Liver transplant surgery is a complex and delicate procedure that requires a highly skilled surgical team and meticulous postoperative care.
What happens immediately after the liver transplantation or what is post transplant care?
Postoperative care after liver transplantation is crucial to ensure the patient’s well-being and the success of the transplant. Here are some key aspects of postoperative care:
Initially, the patient is closely monitored in the ICU to ensure stable vital signs, blood pressure, heart rate, oxygen levels, and urine output. This allows medical professionals to detect any complications early on.
To prevent organ rejection, the patient will be prescribed immunosuppressive medications, such as steroids, tacrolimus, cyclosporine, or mycophenolate mofetil. These medications suppress the immune system to prevent it from attacking the transplanted liver. Compliance with the medication regimen is crucial.
Transplant recipients are at increased risk of infections due to immunosuppression. Strict infection control measures, such as hand hygiene, aseptic techniques during dressing changes, and prophylactic antibiotics, are implemented to minimize the risk of infections.
Regular monitoring of liver function is performed through blood tests, including liver enzymes, bilirubin, and immunosuppressant drug levels. This helps evaluate the function of the transplanted liver and adjust medication dosages if necessary.
Maintaining proper fluid and electrolyte balance is essential. Intravenous fluids may be administered initially, and oral intake is gradually increased. Electrolyte levels, such as sodium, potassium, and magnesium, are closely monitored and supplemented as needed.
Proper nutrition is crucial for healing and recovery. A registered dietitian works with the patient to develop an individualized nutrition plan, considering the patient's dietary preferences and any specific needs or restrictions.
Gradual mobilization and physical activity are encouraged to prevent complications such as blood clots and pneumonia. Physical therapists may assist with exercises and help the patient regain strength and function.
Liver transplantation can be emotionally challenging for patients and their families. Psychosocial support, including counseling, support groups, and assistance with managing stress and anxiety, can be provided to help patients cope with the transplant process.
Regular follow-up appointments are scheduled to monitor the patient's progress, adjust medications, and detect any signs of complications or rejection. These appointments may involve blood tests, imaging studies, and consultations with the transplant team.
How is the follow up care done after discharging from the hospital?
Follow-up care after liver transplantation is crucial for the long-term success of the transplant and the overall well-being of the patient. Here are some key aspects of follow-up care:
Patients are scheduled for regular follow-up visits to the transplant clinic. Initially, these visits may be frequent (e.g., weekly or monthly) and gradually become less frequent as the patient’s condition stabilizes. During these visits, the transplant team evaluates the patient’s overall health, monitors liver function, and assesses the status of the transplanted liver.
Blood tests are performed during follow-up visits to monitor liver function, assess the levels of immunosuppressive medications, and check for any signs of rejection or complications. These tests typically include liver enzymes, bilirubin, creatinine, complete blood count (CBC), and immunosuppressant drug levels.
In selected patients imaging studies, such as ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI), may be conducted to evaluate the structure and function of the transplanted liver, detect any abnormalities or complications, and monitor the status of blood vessels and bile ducts. These tests are selectively done and not routinely done in all patients.
The patient’s medication regimen, including immunosuppressive medications, is regularly reviewed and adjusted as needed. The transplant team closely monitors medication levels, side effects, and potential drug interactions. Adherence to the prescribed medication schedule is crucial to prevent rejection and ensure the long-term success of the transplant.
Transplant recipients may require specific vaccinations to protect against infections. The transplant team will provide guidance on recommended vaccines and the appropriate timing for administration, taking into consideration the patient’s immunosuppression status.
The patient’s dietary needs and restrictions are regularly evaluated and adjusted as needed. A registered dietitian may provide guidance on maintaining a balanced diet, managing weight, and avoiding foods that may interact with medications or pose a risk to the transplanted liver.
The transplant team educates patients on the signs and symptoms of rejection, such as fatigue, jaundice, abdominal pain, or changes in liver function. Patients are instructed to report any concerning symptoms immediately to their healthcare provider.
Patients and their caregivers are educated about self-care practices, including medication management, infection prevention strategies, the importance of a healthy lifestyle, and recognizing and managing potential complications. Education empowers patients to actively participate in their own care and promotes a successful long-term outcome.
Follow-up care after liver transplantation is typically provided by the surgical team. The frequency and duration of follow-up visits may vary depending on the patient’s progress and individual needs. It is important for patients to maintain regular communication with their transplant surgeon and adhere to the recommended follow-up schedule to optimize their post-transplant outcomes.
What are the signs and symptoms of rejection?
Rejection after liver transplantation is less common and less severe compared to other organ transplantation and it can be reversed with simple medicines. Rejection does not always cause noticeable symptoms. In fact it is commonly detected in routine blood tests. As such, it’s very important not to miss regularly scheduled appointments with your doctor. If there are symptoms, each individual may experience them differently. Some of the more common signs and symptoms of rejection include:
- Fever
- Headache
- Fatigue
- Nausea
- Loss of Appetite
- Itchy Skin (pruritus)
- Dark-Colored Urine
- Jaundice (a yellowing of the skin and whites of the eyes)
- Abdominal tenderness or swelling
How is transplant rejection treated?
Acute liver rejection may occur in up to 10% of liver transplant recipients and most of them can be reversed. It’s most common within the first three months after transplantation, but can occur at anytime. To prevent rejection, you must take immunosuppressive medications for the rest of your life. These may include:
- Prednisone
- Tacrolimus
- Cyclosporine
- Sirolimus
- Mycophenolate mofetil

The dose of these medications may change frequently, depending on your response. Generally, you can expect to take more medications the first few months following transplantation after which time some may be discontinued or the doses lowered. The goal is to maintain a balance between preventing rejection and making you susceptible to infection and other side effects associated with the long-term use of immunosuppressants.
What is the long-term protocol after liver transplantation?
People usually return to normal activities 3 months following transplantation. Frequent visits and intensive medical follow-up with the transplant team are essential during the first three months. To achieve the best outcome, it’s important for you to be an active participant in your own healthcare
- Keep all medical appointments.
- Take medications exactly as prescribed
- Learn the signs of rejection and infection and report them promptly to your healthcare provider.
- Avoid people who have a contagious illness (colds, flu, etc.).
- Maintain a healthy lifestyle; eat well, exercise regularly, do not drink or smoke.
- Avoid dust and crowded places.
- Avoid pets and direct handling of soil.










